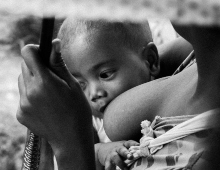
Breastfeeding is one of the most cost-effective interventions for improving the health and survival of children, with important short and long-term benefits to families and society. However, policies and interventions to support breastfeeding are undermined by powerful multi-national formula milk manufacturers who compete for a share of infant feeding.
The Code of Marketing of Breastmilk Substitutes (BMS Code) including subsequent World Health Assembly resolutions, is an attempt to counter harmful marketing of breastmilk substitutes to the public and health professionals. But enforcement is weak and code non-compliant marketing continues despite BMS Code-related legislation.
In the field of child health and nutrition, the primary responsibility of health professionals is to safeguard optimal health and development, which includes protection and support of breastfeeding. The primary concern of companies who manufacture breastmilk substitutes is profit, and their marketing strategy often targets endorsement by health professionals. The intersection of these two groups therefore leads to conflicts of interest.
In February 2019, a bold decision by the UK Royal College of Paediatrics and Child Health to halt funding from manufacturers of breastmilk substitutes has once again highlighted a long-ignored conflict of interest and been followed by other decisions such as that of The British Medical Journal to no longer carry advertisements from breastmilk substitutes manufacturers.
But in our view, as academics and child health advocates, more needs to be done to raise awareness about conflict of interest and enforce the code in research, service, training and policy spaces. We call for bold, proactive leadership to eliminate this conflict of interest, especially in low-and-middle income countries with the largest current growth in formula milk sales. A look at the history of breastfeeding protection in South Africa highlights the importance of eliminating these competing interests.
South Africa, an upper-middle income country with discrepantly high levels of young child mortality, has had a complex history in the promotion and support of breastfeeding. In the early 2000s at the height of the HIV epidemic, the Department of Health recommended that women living with HIV should not breastfeed and instead provided six months of free formula milk. With increasing evidence of a negative impact on the health of HIV-exposed infants, suboptimal child mortality reduction and evidence that antiretroviral therapy prevents breastfeeding transmission, national policy evolved to promote breastfeeding by women supported on antiretroviral therapy.
Since 2011, South Africa has scaled up lifelong antiretroviral therapy for women living with HIV and has discontinued free formula milk. In 2012, the code of marketing of breastmilk substitutes was enacted as Regulation 991 with accompanying guidelines for industry and health care personnel. Since 2015, the University of Cape Town’s Department of Paediatrics and Child Health Advocacy Committee and the South African Civil Society for Women’s, Adolescents’ and Children’s Health have monitored and reported contraventions of Regulation 991 by breastmilk substitutes manufacturers. These have included offers to sponsor academic positions within universities, industry exhibition stands advertising specialised formula milks and sponsored breakfast symposia at paediatric, nutrition and allergy conferences and hosting of continuing medical education symposia for nurses and dieticians.
These are not a few isolated cases but rather part of a global phenomenon with a series of recent reports documenting persistent, systematic violations by the breastmilk substitutes industry. There is also a WHO report concluding that “Protecting the health of children and their mothers from continued misleading marketing practices should be seen by countries as a public health priority and human rights obligation”.
These examples illustrate the need to eliminate conflict of interest among health professionals and institutions focused on children’s health. South Africa has fought a long, hard battle to protect, promote, and support breastfeeding. Policy decisions and programme implementation helped to increase the exclusive breastfeeding rate from 8% to 32% but it still falls far short of the Global Nutrition Target of 50% by 2025. Moreover, the extensive use of formula milk (27% of infants aged 2-3 months) is particularly concerning when 66% of infants live in households below the upper-bound poverty line and 30% lack potable water on site, with consequent vulnerability to diarrhoea and pneumonia.
Globally, 136 out of 194 countries have code-related legislation, yet contravention and violations persist in the face of weak monitoring and enforcement mechanisms. Internal review and disclosure, and proactive policies by institutions involved in child health policy, research, training and service to identify and counter breastmilk substitute-related conflict of interest is urgently required to send a clear message to industry. The recent bold decisions by the Royal College of Paediatrics and Child Health and The British Medical Journal will hopefully spark similar action in professional bodies and universities in low and middle-income settings. These institutions, who are important thought leaders, need to act independently and with integrity in the best interests of children.